Interventions
Hallux Valgus
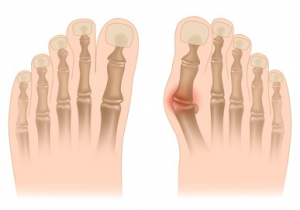
The most common deformity is HALLUX VALGUS (commonly called the "bunion"). It affects the first ray of the foot, where the phalanges are deviated outward and the first metatarsal is deviated inward.

Hallux Rigidus
Hallux rigidus is the name given to primary osteoarthritis of the first metatarsophalangeal joint, as well as between the head of the first metatarsal and its sesamoids.
Hallux Valgus
The most common deformity is HALLUX VALGUS (commonly called the "bunion"). It affects the first ray of the foot, where the phalanges are deviated outward and the first metatarsal (the long bone on the inner edge of the foot) is deviated inward.
Hip
Hip wear is often accompanied by reduced joint amplitude (stiffness) and, above all, pain.
Knee
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Hallux Valgus
In Brief
This is a deformity of the big toe, often called a "bunion", which can cause a painful bump on the side of the foot. If left untreated, this deformity can lead to further pain and affect the other toes.
Causes
Hallux valgus is often linked to hereditary factors, unsuitable footwear or aging. Sometimes, trauma or certain illnesses may be responsible.
Intervention
Correction is performed through a small incision, allowing rapid recovery and discreet scarring.
Recovery
After a short hospital stay, a dressing is maintained for about 3 weeks to ensure correction. Walking is gradually resumed.
Hallux Valgus
What's it all about?
La déformation la plus fréquente est l’HALLUX VALGUS (communément appelé «l’oignon»). Elle concerne le premier rayon du pied dont les phalanges sont déviées vers l’extérieur et dont le premier métatarsien (os long du bord interne du pied) est dévié vers l’intérieur.
This deviation is responsible for a progressive dislocation of the metatarsophalangeal joint. The head of the first metatarsal becomes subcutaneous, giving the impression of a "growing bump" whose volume is increased by the frequent association of bursitis (a pocket of subcutaneous inflammation). This deformity is responsible forable to cause pain on the inside edge of the foot when walking and deformity of footwear.
When deformity is left untreated, it is not uncommon to see the appearance of METATARSALGIA which are the consequence of the heads of the lateral metatarsals (long bones of the foot) being too long in relation to the first radius.
Advanced hallux valgus is often accompanied by an impact on the lateral toes in the form of PHALANGEAL CLAWS.
In the absence of regular podiatry care, the following symptoms may appear DURILLONS(skin thickening) on the toes due to dorsal impingement when putting on shoes, or plantar calluses under the metatarsal heads due to excessive weight-bearing.
When they are not too troublesome, deformities can be treated with appropriate footwear and custom-made orthopedic inserts. However, these measures are not curative, but only symptomatic, i.e. they may reduce pain but do not eliminate or halt the long-term trend towards aggravation.
When deformities accelerate and become uncomfortable to walk on, or deform the shoe, they can be surgically corrected.
Numerous surgical techniques are available. They are all based on essentially bony procedures (OSTEOTOMIES), but also gestures on ligaments and tendons (soft tissue).
Causes of the disease
Several factors may overlap.
The female sex is most often affected. Genetic factors have also been suggested, so there is a hereditary component. This heredity is not observed by a deformity from birth, but by predispositions to foot "morphotypes" that are potentially deformable. These are so-called "Egyptian" or "Greek" forefeet, where the big toe is respectively too long or too short in relation to its neighbor. In addition, the arch of the foot may be deformed into a flat foot, or the ankle and knee into "valgus".
Shoe type acts as a catalyst, accelerating deformations. Ill-fitting shoes, especially those with high heels and narrow "toes", contribute to the earlier onset of the disease. Trauma (sprain, dislocation, foot fracture) can sometimes reveal a previously well-tolerated deformity.
In some cases, a neurological or rheumatological disease may be the cause. responsible.
Finally, with age, ligaments become more elastic, and deformities that have long been tolerated become more pronounced, sometimes suddenly, within a few months. These phenomena are often concomitant with menopause in women, but also appear in men at an older age. Despite all these causes, there may be no obvious reason for the deformity.
What does the operation involve?
The operation is performed using the minimally invasive called percutaneous. This means that all surgical procedures are performed through the skin, without "opening". However, the skin barrier is penetrated to the width of the instruments required for bone or soft tissue procedures (burs, blades). As a result, scars are usually less than 5 mm long.
The surgeon uses an X-ray machine to take X-rays during the operation. This enables him to know where he will be making an osteotomy or correcting a deformity.
Percutaneous surgery offers many advantages. In addition to do not produce large scarsit allows you toavoid tissue detachment extensive. The technique enables do without equipment The use of osteosynthesis devices (screws, pins, staples, plates, etc.) to fix osteotomies means that no foreign bodies are left in the foot. This reduces the risk of infection. Finally, the bone powder produced during osteotomies is used as a natural graft helping your own body to produce more rapidly a bone callus which will consolidate or "harden" the bone once corrected.
Open techniques exist, but require the use of hardware to fix the bone. There are also hybrid techniques in which screws are inserted through small incisions. These other techniques have their advantages and disadvantages. Each surgeon uses the technique he or she has learned or developed best, in line with the latest scientific findings.
Hospitalization
In most cases, you will be hospitalized on an outpatient basis. Conventional hospitalization is also possible if the medical and social context so requires. Anesthesia can be spinal (such as an epidural), general or locoregional. The decision is taken with you, during the pre-operative consultation with the anaesthetist.
Once the operation is over, you return to your room after a short period of observation in the recovery room. You will be shown how to walk in your off-loading shoe and how to use the cryotherapy bags, which are highly effective against pain and swelling.
You go home (accompanied by a relative or by taxi/ambulance if no one is available to pick you up) with the dressing made in the operating room by your surgeon. This dressing is to keep dry, without changing ituntil around the 21st postoperative day. Single-stage bilateral surgery should be avoided, as it complicates the management of autonomy and pain, and increases the risk of phlebitis. It is still possible, however, if an interval of 2 to 3 weeks is observed between each side.
What happens after the operation?
Given the absence of material to fix osteotomies, dressing plays an essential role. It is applied in the operating room by your surgeon. It enables the toes to be fixed in a corrective position imposed by the bandages, until the bone callus appears.
The dressing does not need to be removed for the first 3 weeks, and will be removed by a homecare nurse around the 21st post-operative day, a few days before the follow-up visit, which is usually at one month.
Compression of the osteotomies by the dressing can give the appearance of overcorrection or strangulated toes. This may seem impressive, especially when the bandage is removed at home. Don't worry, it's normal and voluntary, especially the spread of the big toe which, if initially insufficient, can lead to an early recurrence. These factors are not cause for concern, and will return to normal once the dressing and medical shoe have been weaned off, around the 6th post-operative week.
Support is protected for the first 4 weeks by a rigid-soled shoe. Canes are not usually required to wear this shoe, but they will be prescribed so that you can walk in it with confidence, if necessary. The shoe is prescribed to you as soon as the operation is scheduled, so that you can practice putting it on and wearing it at home the week before the operation.
Post-operative, alternating walking and elevation is recommended of the operated foot, as often as possible (foot on a cushion in bed, foot on a chair in a sitting position, foot on the back seat of a car, etc.) with the knee in extension. A downward position (foot down) or a knee bent for a long period of time can cause swelling, which can increase pain and make the dressing too tight. The operated foot should be supported regularly, for 5 to 10 minutes every half-hour. This not only stimulates the bone for better healing, but also reduces the risk of phlebitis and enables you to remain independent, even when climbing stairs.
Anti-coagulant treatment is systematically prescribed for the first 14 days post-op to prevent phlebitis.
From the 5th week, free shoeing can usually be resumed. Resumption of walking is a gradual process, as shoeing is not always immediate due to swelling, which varies from patient to patient. Self-education exercises will be suggested, possibly in conjunction with physiotherapy sessions.
The swelling may increase after the dressing has been removed, in which case you will be offered compression socks. To avoid a partial recurrence of the deformity when you return to your shoes (which are inevitably too tight at first), you will be asked to wear a toe spreader for several weeks.
Resumption of work varies according to the extent of the deformity to be corrected and your occupation. It generally takes place between 1 and 2 months after the operation. While the medical shoe is being worn, driving is not recommended, due to the rigidity of the sole and the thickness of the dressing. Once the dressing has been removed, you may be able to slip on a soft, loose shoe while driving, but the shoe must be kept on for walking until the end of the 4th post-operative week.
Once the post-operative oedema has subsided, you will be prescribed a pair of orthopedic insoles to help the foot regain homogeneous support while it recovers natural plantar support. These will generally be worn for a year after the operation.
FAQ
Foot infection
Foot infection has become rare with the advent of percutaneous techniques. However, the risk is increased when there are other associated diseases such as diabetes or arteritis. Smoking is also an additional risk factor.
Phlebitis
Phlebitis is prevented by anti-coagulant treatment, and should be detected if calf pain occurs by an ultrasound Doppler test, which your GP or surgeon may prescribe.
Secondary displacement of osteotomies.
Given the absence of hardware fixation, non-compliance with the medical shoe, early removal (before 20 days) or excessive walking can lead to this complication. In the event of significant displacement, the final result may be compromised.
Algodystrophy
Stiff toes
If the deformities were very significant or long-standing, the flexibility of the toes cannot be restored by the operation. Some toe claws require tendons to be lengthened or, on the contrary, a phalanx to be shortened, resulting in reduced mobility. It is not uncommon for some toes not to touch the ground when they are reloaded, as long as edema persists in the sole of the foot. Your surgeon will suggest a suitable rehabilitation program if you experience any discomfort.
Paresthesias
Edema
Recurrence of the deformity
The appearance of other deformations
Osteoarthritis
Excessive correction
Toe necrosis
The death
This list of complications is intended to inform you, not frighten you. Your surgeon is a professional who proposes an operation to treat a deformity. He or she weighs up the risks and benefits of an operation with you, and you are always free to accept or refuse. Post-operative follow-up allows us to detect any complications and offer you appropriate treatment if necessary.
The aesthetic result may sometimes appear disappointing, but the aim of this surgery is not aesthetic but functional. The main aim of the surgery is to make the foot more wearable and less painful, and to prevent the deformity from progressing to extreme situations which, after a certain age, can no longer be treated by conservative surgery.
Foot surgery is a complex discipline, all the more so when the deformities are old and multiple. Several operations, spread out over time, may be necessary to achieve a satisfactory result.
Consultation
Make an appointment with
Dr. Paul MIELCAREK
Make an Appointment
You can make an appointment with the Doctor directly on Docolib from the Contact page.
Teleconsultation
Visit Consulib to book a teleconsultation appointment with Dr Paul Mielcarek.
Cabinet
5 Rue de la Coopérative, HALL 1, 67000 Strasbourg, welcomes you Monday to Friday, 8am to 12pm and 2pm to 6pm.




